Chapter 19: CPT Evaluation & Management Section Workbook Case 2 Answers and Rationale.
The patient is a 32-year-old male here for the first time. |1|
Chief Complaint: Left knee area is bothersome, |2| painful, moderate severity. The patient also notes swelling in the knee area, limited ambulation, and inability to perform physical activities such as sports or exercises. The patient first noticed symptoms approximately 4 months ago. Problem occurred spontaneously. Problem is sporadic. Patient has been prescribed hydrocodone and meloxicam. Patient has had temporary pain relief with the medications. The meloxicam has caused digestion problems so patient has avoided using it.
Past Medical History: Patient denies any past medical problems.
Surgeries: Patient has undergone surgery on the appendix.
Hospitalizations: Patient denies any past hospitalizations that are noteworthy.
Medications: Hydrocodone.
Allergies: Patient denies having allergies.
Family History: Mother: No serious medical problems; Father: No serious medical problems.
Social History: Patient is married. Occupation: Patient is a chef.
Review of Systems:
Constitutional: Denies fevers. Denies chills. Denies rapid weight loss.
Eyes: Denies vision problems.
Ears, Nose, Throat: Nose, Throat: Denies any infection. Denies loss of hearing. Denies ringing in the ears. Denies dizziness. Denies a sore throat.
Denies sinus problems.
Cardiovascular: Denies chest pains. Denies an irregular heartbeat.
Respiratory: Denies wheezing. Denies coughing. Denies shortness of breath.
Gastrointestinal: Denies diarrhea. Denies constipation. Denies indigestion. Denies any blood in stool.
Genitourinary: Denies any urine retention problems. Denies frequent urination. Denies blood in the urine. Denies painful urination.
Integumentary: Denies any rashes. Denies having any insect bites.
Neurological: Denies numbness. Denies tremors. Denies loss of consciousness.
Hematologic/Lymphatic: Denies easy bruising. Denies blood clots.
Psychiatric: Denies depression. Denies sleep disorders. Denies loss of appetite.
Review of Previous Studies: Patient brings an MRI which is reviewed. |3| Large knee effusion. No lateral meniscal tear. No ACL/PCL tear. No collateral fracture. Medial meniscus tear with grade I signal.
Vitals: Height: 6’0”, Weight: 160
Physical Examination: Patient is alert, appropriate, and comfortable. Patient holds a normal gaze. Pupils are round and reactive. Gait is normal. Skin is intact. No rashes, abrasions, contusions, or lacerations. No venous stasis. No varicosities. Reflexes are normal patellar. No clonus.
Knee: Range of motion is approximately from 5 to 100 degrees. Pain with motion. No localized pain. Negative mechanical findings. There is an effusion. |4| Patella is tracking well. No tenderness. Patient feels pain especially when taking stairs or squatting. |5|
Hip: Exam is unremarkable. Normal range of motion, flexion approximately 105 degrees, extension approximately 10 degrees, abduction approximately 25 degrees, adduction approximately 30 degrees, internal rotation approximately 30 degrees, external rotation approximately 30 degrees.
Neck: Neck is supple. No JVD.
Impression:
1. Infective synovitis of the left knee
2. Contracture of the left knee
3. Possible |6| medial meniscal tear of right knee
Assessment and Plan: A discussion is held with the patient regarding his condition and possible treatment options. Patient has GI upset. |7| Patient is recommended to take Motrin 400 two to three times a day, |8| discussion is held regarding proper use and precautions. Patient is given a prescription for physical therapy. |9| We will obtain an MRI |10| to rule out potential medial meniscus tear. Patient is instructed to follow up with PMD with labs. |11| Patient is referred to Dr. XYZ. Patient may need arthroscopy if patient does have medial meniscus tear and repeat effusion. |12|
|1| This is a new patient.
|2| Chief complaint.
|3| The provider reviews a prior MRI.
|4| Effusion is collection of fluid around the knee.
|5| Pain is a symptom of the final diagnoses and is not reported separately.
|6| This is an undiagnosed new problem. More testing is required to determine the extent of the injury.
|7| GI upset is taken into consideration when providing a plan, although there are no details provided to expand on that or to report it as an additional diagnosis.
|8| Over-the-counter (OTC) medication.
|9| Physical therapy ordered.
|10| MRI ordered.
|11| No indication the labs were ordered or reviewed at this encounter.
|12| Plan for future encounters but not addressed during this encounter.
What are the CPT® and ICD-10-CM code(s) reported?
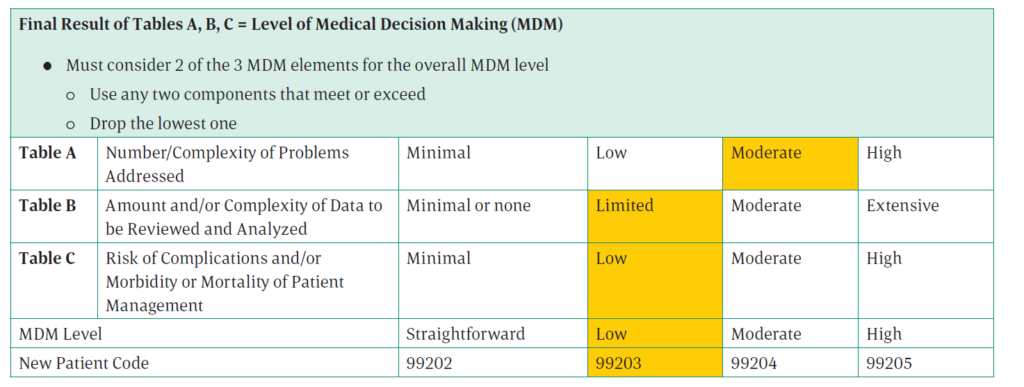
CPT® code: 99203
ICD-10-CM codes: M65.162, M24.562
Rationale:
CPT® code: Subcategory — Office visit, new patient, coded using 2021 E/M guidelines
Number and complexity of problems addressed: One acute, complicated injury, makes this moderate for the number and complexity of problems addressed. The patient has an infection in the knee and could potentially have a torn meniscus.
Amount and complexity of data to be reviewed and analyzed: The provider reviewed a prior MRI (new patient, so the MRI was ordered and performed by another provider) and ordered a new MRI, making this limited for the amount and complexity of data to be reviewed and analyzed.
Risk of complications and morbidity or mortality of patient management: The patient is prescribed OTC medications and physical therapy. The risk of patient management is low.
ICD-10-CM codes: In the ICD-10-CM Alphabetic Index, look for Synovitis/infective NEC, and you are directed to see also tenosynovitis. Look for Tenosynovitis/infective NEC/lower leg referring you to M65.16-. In the Tabular List, 6th character 2 is reported for the left leg. Next, look for Contraction(s), contracture, contracted/joint/knee M24.56-. In the Tabular List, 6th character 2 is reported for the left knee. The medial meniscal tear is only a possible diagnosis, so it should not be coded.
